
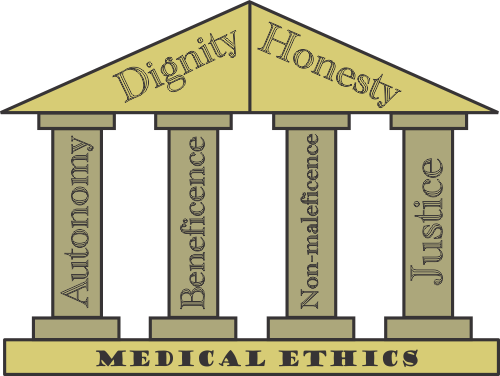
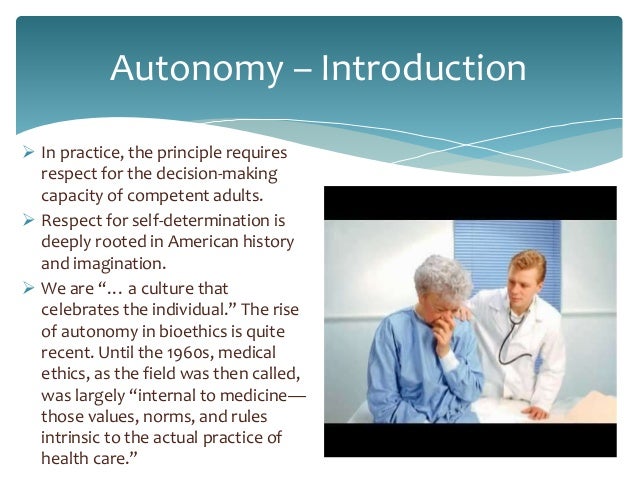
Ethical DilemmaĪn ethical dilemma is a conflict in values that cause distress and controversy, and in the nursing practice this could be for the nurse, the patient, or the patient's family.Īn example of an ethical dilemma you might encounter in your nursing career is: the daughter of an intubated patient with terminal cancer does not want her mother to have opioid pain medication due to religious reasons, even though she is in severe pain. For example, if a patient was starting chemotherapy and asked about the side effects, a nurse practicing veracity would be honest about the side effects they could expect with chemotherapy. Veracity means to tell the truth-to never lie to patients or give them knowingly false reassurance, which is also lying. For example, a nurse who told their patient they were coming back in 30 minutes to check on their pain, would either come back, or delegate somebody else to come back if they got tied up. In nursing, the ethical principle of fidelity means to be faithful or loyal, which means that you keep promises to patients. Nurses practicing in a just manner provide care equally amongst their patients. Nurses practicing justice do not provide care to patients differently based on their race, gender identity, sexual orientation, or religion. For example, if you were juggling multiple patients, you would not provide better care based on who has the best insurance. In nursing, the ethical principle of justice means to treat fairly. The difference between beneficence and nonmaleficence may seem subtle, but you can remember that beneficence is promoting good and nonmaleficence is avoiding harm by remembering that the prefix mal- means bad (think malnourished, malfunctioning, malpractice, malodorous, Maleficent from Sleeping Beauty…) We created our Medical Terminology flashcards to make breaking down words into their parts easy, so you never have to be confused by an unfamiliar word on an exam! Justice For example, a nurse demonstrating nonmaleficence would perform multiple checks before administering medication to avoid a dangerous medication error. In nursing, the ethical principle of nonmaleficence is to avoid causing harm. For example, if a patient has been in the hospital for weeks, a nurse showing beneficence might take that patient outside for some fresh air. In nursing, the ethical principle of beneficence simply means to promote good. For example, a nurse practicing advocacy would notify the provider about a concerning change in a patient's condition. In other words, nurses must advocate for their patients' best interest. In nursing, the ethical principle advocacy is to promote and protect the patient's rights, health, and safety. For example, a patient has a right to refuse treatment. In nursing, the ethical principle autonomy is a patient's right to make their own healthcare decisions. State Boards of Nursing are governmental agencies that set laws for nursing practice, while the American Nurses Association is a non-governmental organization that establishes ethics for nursing practice. What is the difference between the State Board of Nursing and the American Nurses Association?
Ethical principle of autonomy in nursing professional#
The American Nurses Association (ANA) is a professional organization to advance and protect the progression of nursing, and they are the group that establishes the ethical standards of care for the nursing profession.
Evidence-based practice is choosing nursing actions and interventions based on peer-reviewed data that show those actions to be beneficial for patients.Įvidence-based practice is an important concept for nursing that will feature heavily in your nursing education-you may even take a class in it. Evidence-Based PracticeĮvidence-based practice means using the best data and evidence from research to guide nursing practice.Įvidence-based practice means not doing something just because that's the way it has always been done, or because it's easier for the nurse. If you practice nursing in multiple states, you will be required to know what your scope of practice is in each state. A scope of practice is what a nurse is allowed to do with their licensure (e.g., RN, PN) in a given state. The Nursing Practice Act is a document outlining a set of laws that defines qualifications for licensure, nursing titles, and a nurse's scope of practice. Nursing Practice ActĮach state has a Nursing Practice Act set forth by its State Board of Nursing. NCLEX exams are also developed and owned by the NCSBN. In the US, all of the State Boards of Nursing together make up the National Council of State Boards of Nursing (NCSBN).
Each state's State Board of Nursing governs nursing licensure requirements for the state.

Every state in the US has a State Board of Nursing.


 0 kommentar(er)
0 kommentar(er)
